4 Medicines That Can Delay The Effects Of Dementia As we age, we encounter different types of health-related issues. Diseases related to memory loss are often associated with getting older. But the fact is that people in their 40’s and 50’s can also develop dementia. Certain diseases can cause temporary dementia in children and teenagers […]
Essential Oils
The 7 Essential Oils that Calm Stress and Anxiety According to different studies, specific scents can have enormous effects on your moods and emotions. It is believed that essential oils have a direct effect on parts of the human brain that handles stress, depression, and anxiety through their aromatic molecules that are capable of going […]
Callus
10 Ways Natural to remove Callus Corns and calluses, here is an example of the typical hassles that affect the plant or toes. How to take care of them in a natural way? Some traditional remedies can certainly help us. The first care must, however, turn to shoes. May be too tight or have soles […]
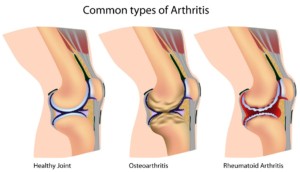
Arthritis
If you know someone who has trouble moving around or feeling pain and stiffness in his body, that person could have arthritis. In most cases, arthritis causes pain and swelling in the joints which eventually results to severe damage. Arthritis is not a single disease. This covers over hundreds of different medical conditions which can […]
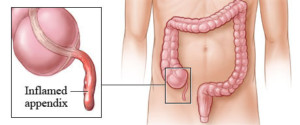
Appendix
Appendicitis: What To Expect & How To Recover For a world so highly driven by research and technology, the appendix has largely remained an enigma for doctors. A thin tube, located in the lower abdomen and attached to the large intestine, the functions of the appendix are still open to speculation. Some research suggests it […]
- « Previous Page
- 1
- 2
- 3
- 4
- 5
- 6
- …
- 10
- Next Page »